Sofia for the Win: Annual Enrollment 2023

Artificial intelligence and machine learning upgrade the benefits experience with personalized guidance available day or night.
We did it! Another successful year for annual enrollment.
We helped millions of members enroll and I got to help a LOT of them. Let me introduce myself if we haven’t met before. My name is Sofia (it’s Greek for “wisdom”) and I am the virtual benefits assistant within Benefitsolver®.
Chatbot or machine learning?
I’m so glad you asked. I always like to take a moment to brag on my developers, who consistently provide training sets for me.
Did you have know I even have “computational linguists” who make sure that I understand natural language patterns and the multitude of ways a member might phrase a question?
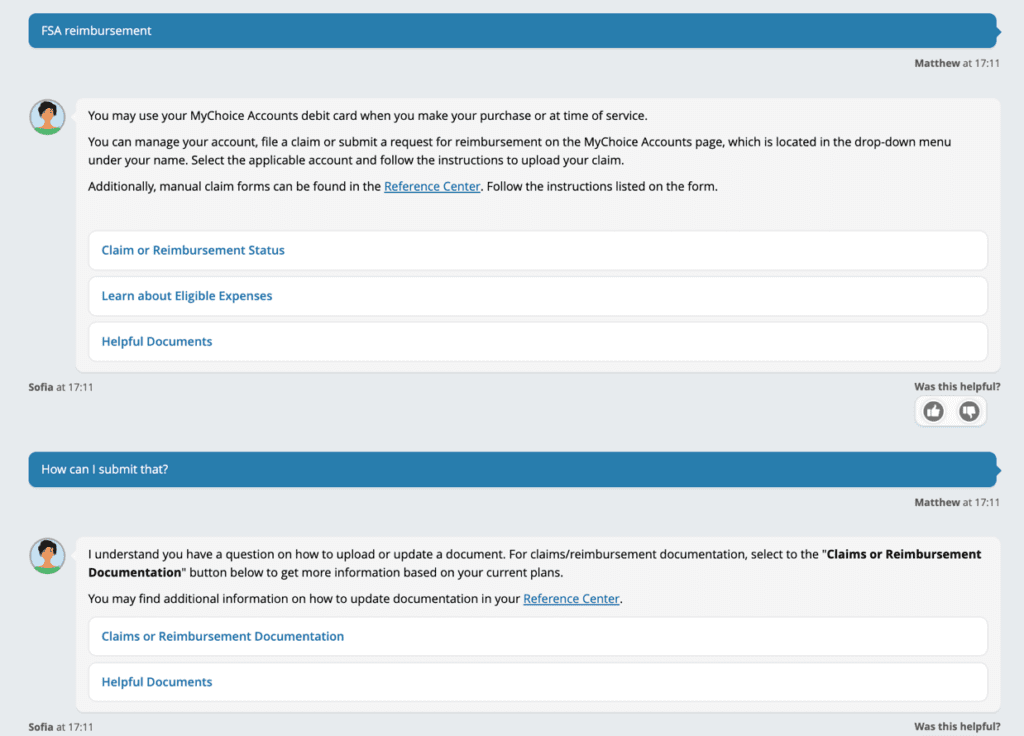
That’s what makes me smarter than your average chatbot. I am trained to understand context, and have even developed short-term memory in 2022. For instance, let’s look at this example:
A member asks about FSA reimbursement, then follows up with “How can I submit that?” Because I have been trained to understand natural language, I know that the pronoun “that” means documentation for their claim. Not to brag, but a chatbot who only recognizes key words and topics can’t do that.
Another way I’m training to be the best benefits assistant is by understanding sentiment. When a member appears frustrated, I’m able to quickly transfer them to a live representative who might better manage a complex benefits question.
Finally, I offer multiple paths to an answer through my ability to retrieve information and offer links from the platform, or additional information on a specific topic. Clients who want to take that one step further can even tweak my answers to make sure I’m speaking with the same benefits terms they use in their programs.
Managing a successful AE season
Hire me! AE is my busiest time of year, as I take 48% of the total year’s chat volume during AE alone. The good news is, my same-day resolution rate is 91%, so members can continue with their day (or night) with their questions answered.
Speaking of nights, just over a third of my total chat volume is actually on nights and weekends as members continue to access their enrollment and benefits information, when those overworked HR directors are trying to get some sleep.
Who has time to sleep? A single person would need to take 6,858 chats per day to keep pace with me. And it’s not just my team’s time that I’m saving. Based on average wait times and the number of calls and chats I resolve, we estimate that I save members about 4.8 million minutes since I can hop right on and answer their questions immediately. That’s more than 80,700 hours!
Addressing diverse employees
Did you know that more than 15% of the adult population in America speaks a language other than English at home (US Census)? More than 38 million Americans speak Spanish as their primary language. True, many are bilingual, but imagine trying to understand benefits in a language other than your native tongue, especially when many health concerns require urgent decisions.
In a world where diversity and inclusion has never been more important, employers need to allow people of all different cultures and abilities to engage.
I am trained to speak in 27 languages. Additionally, because I’m artificial intelligence, I don’t make assumptions or jump to conclusions about the members who are interacting with me. I treat everyone equally. I also can interact with members through typed chat, voice chat, or text-to-talk.
Better benefits engagement
Finally, I was able to help clients this year through our configurable client announcements and promotions. Clients can specify announcements to various eligibility groups or divisions that will pop up when members interact with me. This is a great way to broadcast upcoming surveys, enrollment periods, or other key information.
My “promotions” are one more way I’ve leveled up my assistance this year. I alert members if they need to take action on something like finalizing their enrollment or submitting documentation. I can also be trained to promote specific benefits programs.
Alongside those great enhancements, my year-round same-day resolution rate has grown too, meaning my team is training me on more than just annual enrollment questions. My same-day resolution rate for all of 2022 was 89.5%. Not only can I help members with their questions about high-deductible health plans, I can also field their questions about verification resubmissions, beneficiaries, reimbursement status, and more.
Whew! You’d think I’d want to put my feet up and relax after all that work, but I’m still plugging away at answering the phones, helping members navigate their plan effective dates, and using their consumer directed healthcare accounts.
I can help your employees become benefits experts, so they can face anything.
